Best Core and Stretching Exercises for Slipped Disc Patients
What is a slipped disc?
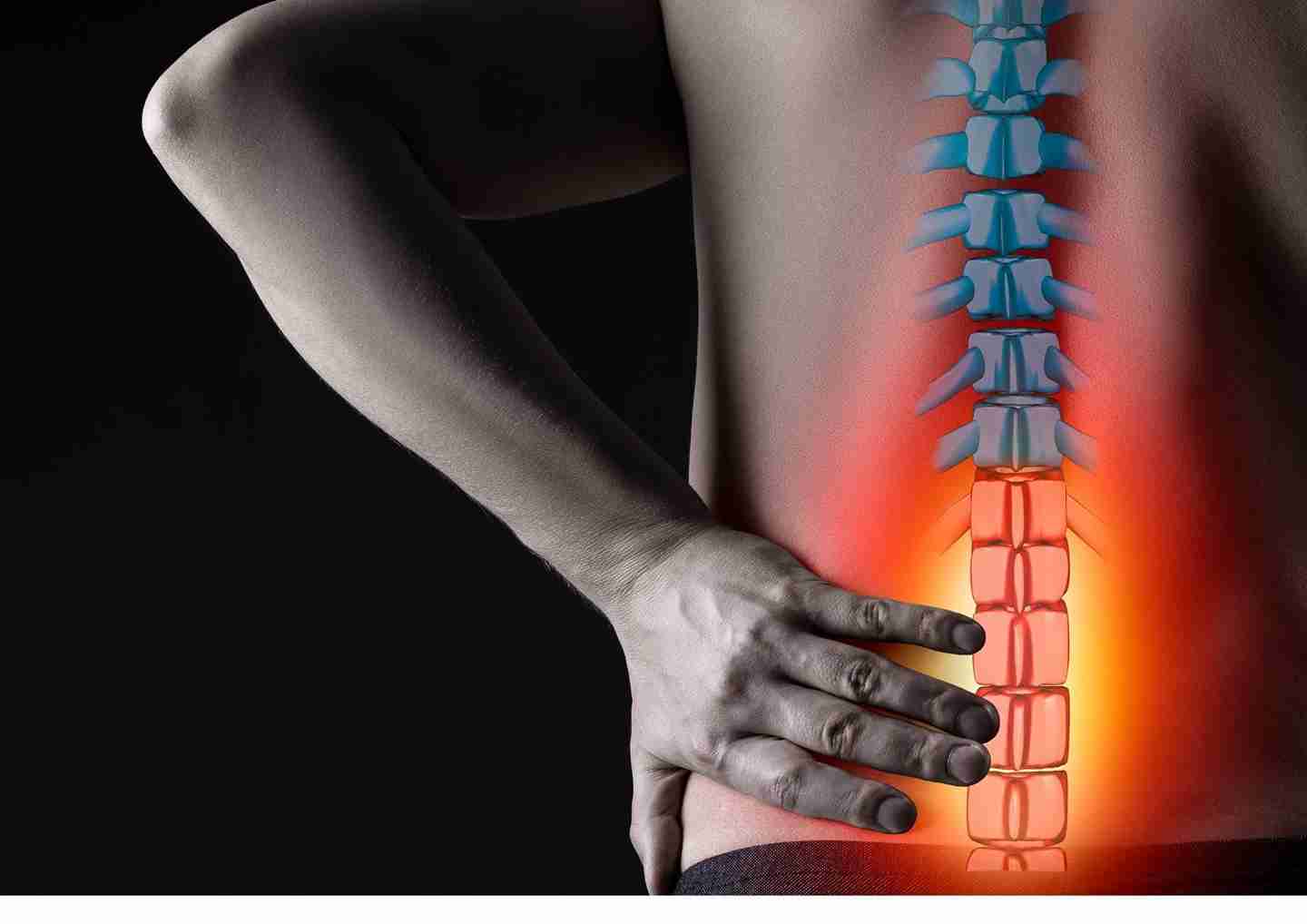
A slipped disc, also known as a herniated or prolapsed disc, occurs when the soft center of an intervertebral disc bulges through its tough outer layer, often causing pain and nerve compression. Common causes include aging, poor posture, heavy lifting, and a sedentary lifestyle. Risk factors like smoking, obesity, and occupational stressors further contribute to disc degeneration.
Symptoms range from sharp, radiating pain and numbness to muscle weakness and mobility issues, depending on the affected nerve. For lumbar discs, pain may extend from the lower back to the legs (sciatica), while cervical issues can impact the arms and shoulders. Severe cases may cause neurological deficits or chronic pain, affecting quality of life.
Physiotherapy for slip discs including targeted core strengthening and stretching exercises, plays a crucial role in managing symptoms, improving mobility, and preventing further complications.
Effective Core and Stretching Exercises for Slipped Disc Recovery
For slipped disc patients, physiotherapy for slip disc such as low-impact exercises are crucial for alleviating pain, enhancing flexibility, strengthening core muscles, and supporting recovery while minimizing the risk of further injury.
Below is a set of recommended exercises:
Stretching Exercises for Pain Relief and Flexibility
Cat-Camel Stretch
- Gently mobilizes the spine and relieves stiffness.
- How to Do It: Start on your hands and knees. Alternate between arching your back upward (cat) and dipping it downward (camel) in a controlled manner.
Child’s Pose
- Relaxes the lower back and decompresses the spine.
- How to Do It: Sit back on your heels, stretch your arms forward, and gently press your chest toward the floor.
Hamstring Stretch
- Reduces tension along the sciatic nerve, particularly helpful for lumbar herniation.
- How to Do It: Sit or lie down with one leg straight and gently pull the opposite leg toward your chest while keeping the back relaxed.
Knee-to-Chest Stretch
- Eases lower back tension and stretches the lumbar spine.
- How to Do It: Lie on your back, bring one knee at a time toward your chest, and hold for a few seconds.
Hip Rolling Stretch
- Improves spine and hip flexibility, relieving pressure on the discs.
- How to Do It: Lie on your back with knees bent and feet flat on the floor. Slowly rock your knees side to side while keeping your shoulders grounded. Perform this motion gently to avoid discomfort.
Core-Strengthening Exercises for Spinal Stability
Pelvic Tilt
- Strengthens the lower abdominal muscles and reduces spinal pressure.
- How to Do It: Lie on your back with knees bent, flatten your lower back against the floor by tightening your abdominal muscles, and hold for a few seconds.
Bird-Dog Exercise
- Enhances core stability and balance.
- How to Do It: Start on your hands and knees. Extend one arm and the opposite leg simultaneously, hold for a few seconds, then switch sides.
Partial Crunches
- Strengthens the abdominal muscles while minimizing stress on the spine.
- How to Do It: Lie on your back with knees bent. Lift your shoulders slightly off the ground, keeping your hands behind your head or crossed over your chest.
McKenzie Prone Press-Up
- Centralizes pain and relieves nerve pressure.
- How to Do It: Lie face down. Place your hands under your shoulders and gently press your upper body upward while keeping your hips on the floor.
Safety Tips for Effective Exercise
- Warm up before starting exercises.
- Avoid high-impact movements or exercises that strain the back.
- Perform each exercise slowly and avoid jerky motions.
- If any exercise increases pain, stop immediately and consult your physiotherapist
Complications of Ignoring a Slipped Disc: Risks and Long-Term Effects
Ignoring a slipped disc and avoiding physiotherapy for a slipped disc can lead to serious complications that significantly impact quality of life. Without proper treatment, the herniated disc may exert increasing pressure on adjacent nerves, resulting in chronic pain, persistent numbness, tingling, and worsening muscle weakness. Over time, this can hinder the ability to perform basic activities like walking, standing, or lifting. Prolonged inactivity can further contribute to muscle atrophy, particularly in the core and lower back muscles, which are essential for spinal stability. This weakness destabilizes the spine, increasing the risk of further injuries. Chronic nerve compression may also cause permanent nerve damage, leading to irreversible sensory loss, impaired reflexes, or loss of motor control. In severe cases, complications such as cauda equina syndrome may develop, characterized by paralysis, and loss of bladder or bowel function, requiring emergency medical intervention. Additionally, untreated chronic pain and disability often lead to emotional distress, anxiety, or depression, compounding the physical challenges. Delayed treatment also slows the healing process, increases dependency on medications, and raises the likelihood of requiring invasive procedures.
Conclusion
Incorporating these stretching and core-strengthening physiotherapy for slip discs exercises into your routine, along with adopting healthy lifestyle habits such as maintaining proper posture, staying active, and managing your weight, can significantly alleviate slipped disc symptoms. Regular physiotherapy sessions are essential for targeted care and recovery.
For expert guidance, Synapse physiotherapy for slip disc is renowned for effectively treating low back pain and slipped disc issues. Their specialized approach, tailored to individual needs, ensures comprehensive recovery and long-term spinal health. Combining professional care with consistent exercises can improve mobility, reduce pain, and help prevent future injuries.
Tags :

Back & Neck Pain
- Spine & Core Rehabilitation
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Group Class

Sports Injuries
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Shockwave Therapy
- Group Class

Work Desk Injuries

Pre-Post-Surgical Conditions

Scoliosis & Postural Abnormalities

Neurological Conditions

Osteoarthritis & Rheumatism
Joint degeneration and inflammation happens as the human body grows older, but that does not mean our way of life degenerates as well. Relief your joint pains with a joint effort together with your physiotherapist, who will provide pain-relief treatments and prescribe exercises for your wellbeing.

Conditions Relating To Elderly
Common conditions in the older age population include hips & knee pain, back & neck pain, osteoarthritis, rheumatism, fear of falling and many more. Aging and degeneration of bodily function is inevitable, but here at Synapse, we will help you live the best of your life.