6 Key Tips to Prevent Work Desk Injuries
Introduction: The Hidden Dangers of Desk Work
Sitting for extended periods during work can negatively impact both physical and mental health. Physically, it often leads to foot pain, swelling, knee discomfort, and muscle tightness, as fluid retention in the legs increases. Prolonged sitting can also contribute to the development of varicose veins and place immense pressure on the spine, resulting in back and neck pain, especially when poor posture is involved. Slouching or hunching over a desk accelerates wear and tear on the spine’s discs, leading to persistent discomfort. Mentally, a sedentary lifestyle is linked to issues such as depression, anxiety, and social isolation, while also increasing the risk of cardiovascular problems like high blood pressure, diabetes, stroke, and high cholesterol. Maintaining good posture, taking regular breaks, and incorporating movement into the workday is essential to minimizing these risks. If you experience any work desk-related injuries, seeking help from a physiotherapist is crucial. You can search for nearby services, such as physiotherapy Ampang, to get professional guidance and treatment.
Common Injuries from Prolonged Desk Work
- Back Pain: Sitting for extended periods often places excessive pressure on the spine and supporting muscles, leading to stiffness, discomfort, and sometimes chronic pain. Poor chair support, improper posture, and lack of movement can exacerbate the issue. Over time, this strain may result in more severe conditions such as herniated discs or sciatica if not addressed.
- Carpal Tunnel Syndrome: This condition occurs when the median nerve running through the carpal tunnel in the wrist becomes compressed due to inflammation. Repetitive wrist movements, improper typing posture, or extended use of a mouse commonly cause it. Symptoms include numbness, tingling, and weakness in the hand, which can make daily tasks challenging if left untreated.
- Eye Strain: Prolonged screen time can cause computer vision syndrome, characterized by blurred vision, dry or watery eyes, headaches, and difficulty focusing. The constant glare, blue light exposure, and lack of blinking during screen use strain the eye muscles. Poor lighting and incorrect monitor positioning can further worsen these symptoms.
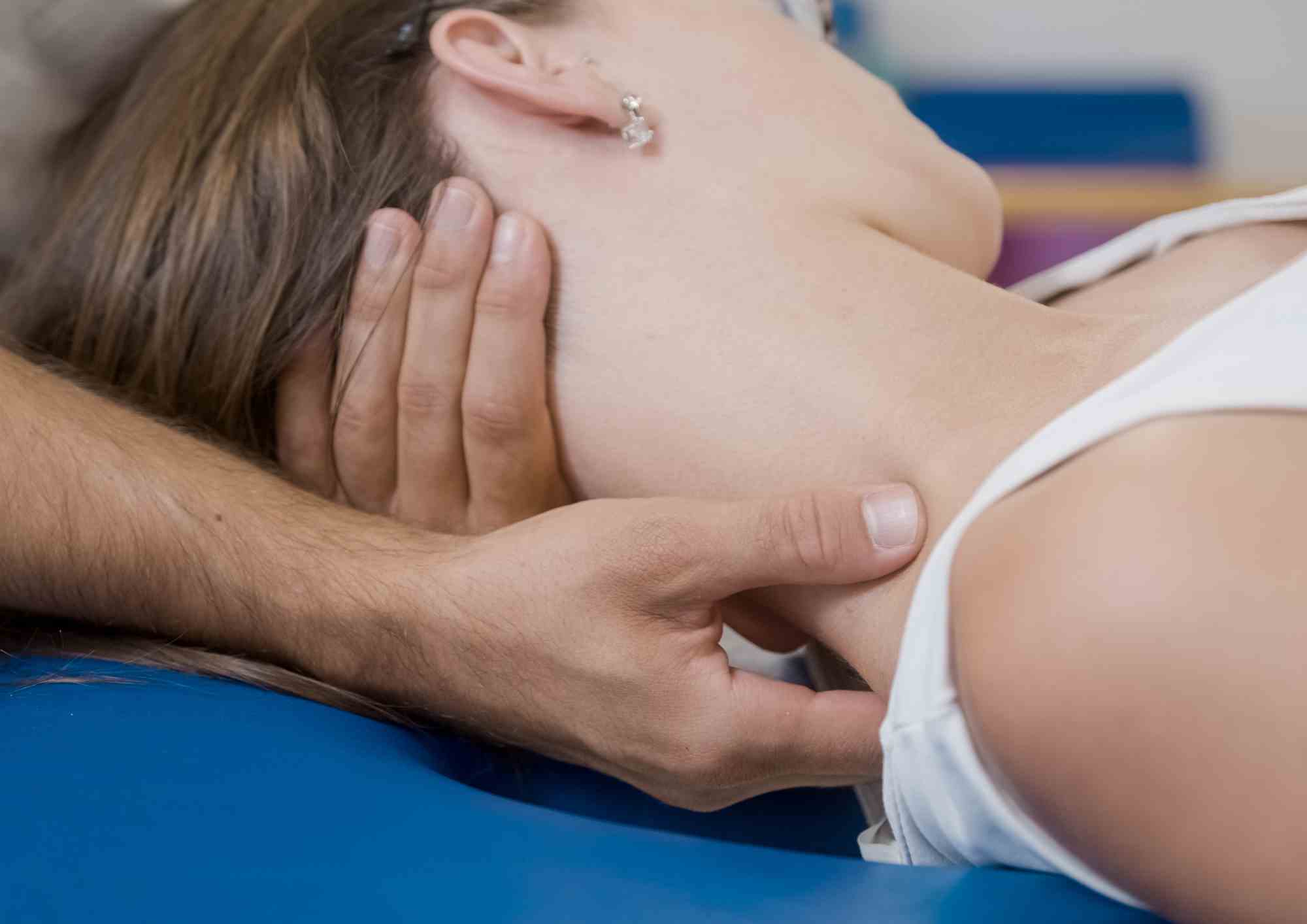
- Neck Pain: Hunching over a desk or craning the neck toward a screen places undue stress on the cervical spine and surrounding muscles. This can lead to stiffness, pain, and reduced mobility in the neck, shoulders, and upper back. Chronic poor posture may contribute to conditions such as cervical spondylosis over time.
- Poor Posture: Using a poorly designed chair or failing to maintain an ergonomic sitting position can lead to habitual slouching or misalignment of the spine. Over time, poor posture weakens the core and back muscles, increasing the risk of muscle imbalances, joint strain, and long-term spinal issues.
- Tendinopathy: Repeated stress on tendons caused by continuous typing, using a mouse, or maintaining awkward postures can result in tendinopathy. This condition involves inflammation, irritation, or microtears in the tendons, leading to pain, stiffness, and reduced strength in affected areas like the hands, wrists, or elbows.
- Repetitive Strain Injury (RSI): RSI develops due to the overuse or improper use of soft tissues, including muscles, tendons, and ligaments. It commonly affects the hands, arms, shoulders, neck, and back. Symptoms include pain, swelling, weakness, and loss of function. Prolonged repetitive tasks, poor posture, or lack of ergonomic equipment are typical causes.
Ergonomics at Your Workstation: Key Tips for a Healthy Workspace
Maintaining proper ergonomics at your workstation is essential for promoting good posture and minimizing the risk of work-related injuries. Here are some key tips to help you set up an ergonomic workspace:
- Chair: Adjust your chair to ensure that it supports your lower back, allowing you to sit upright with your feet flat on the floor. Avoid slouching or leaning forward to reduce strain on your spine.
- Monitor: Position your monitor at or slightly below eye level, ensuring it is about an arm’s length away. If you use multiple monitors, align them at the same height and keep them centered to avoid neck strain from constant head turning.
- Keyboard and Mouse: Place your keyboard close to your body, ensuring that your wrists are straight or slightly angled downward, with your elbows at a 90-degree angle. Keep your mouse next to your keyboard, whether on a separate tray or your desk, to avoid unnecessary reaching.
- Documents: Use document holders to keep paperwork at or near eye level, preventing you from constantly looking down, which can strain your neck.
- Work Surface: Keep your work surface free of clutter, so you don’t have to stretch or reach for items frequently. This helps maintain a natural, relaxed posture while you work.
- Standing: If you have a standing desk converter, alternate between sitting and standing throughout the day. When standing, position precision tasks at or slightly above elbow height, lighter tasks just below elbow height, and heavier work 4–6 inches lower than your elbows for maximum comfort.
- Wrist and Palm Supports: Utilize wrist and palm rests when taking breaks from typing or using the mouse to reduce pressure on your wrists and hands, which can help prevent strain.
By following these ergonomic principles, you can enhance comfort, reduce the risk of injury, and improve overall productivity during long work hours.
Take Breaks
How Often Should You Take Breaks?
Physiotherapy Ampang generally recommends taking a break every 30 minutes, especially for those who spend most of their day sitting or are inactive for extended periods. In addition to shorter breaks, it’s also beneficial to schedule two longer breaks—one in the middle of the first half of the day and another in the second half.
How Long Should a Break Be?
Short breaks of 3 to 5 minutes are typically advised, while longer breaks of at least 10 to 15 minutes can be even more effective in helping to refresh and reduce fatigue.
Posture Matters: How to Sit Correctly at Your Desk
Spine
To prevent spinal strain, sit upright with your upper back straight and your lower back aligned with the chair’s curve. Proper lumbar support is crucial to maintaining the natural curve of your spine, helping to avoid lower back pain, sprains, and conditions like kyphosis (hunchback syndrome) or disc herniation. If your chair lacks support, use a pillow or jacket for added comfort and spinal alignment.
Arms
When your arms are extended forward, it can weaken your upper back, leading to shoulder and back pain. To avoid this, keep your arms at a 90-degree angle and rest comfortably. The arm rests of your chair are designed to provide support, so make sure to use them.
Legs and Feet
To maintain good circulation, avoid crossing your legs, which can restrict blood flow. Position your thighs at a 90-degree angle to your body. If you’re shorter, consider using a footrest to keep your feet flat on the floor and ensure proper blood circulation.
Incorporating Exercise Into Your Daily Routine
Here are some gentle work desk exercises to help relieve tension and improve posture:
1. Neck Stretch
- Sit up straight and slowly tilt your head to one side, bringing your ear towards your shoulder.
- Hold the stretch for 10-15 seconds, then switch sides.
- For a deeper stretch, gently apply pressure with your hand on the opposite side of your head.
2. Trunk Rotation
- Sit upright in your chair with feet flat on the floor and arms crossed over your chest.
- Slowly rotate your torso to one side, keeping your hips stable.
- Hold the stretch for 10-15 seconds, then return to center and repeat on the other side.
3. Seated Forward Bend
- Sit tall with your feet flat on the floor and knees bent at 90 degrees.
- Slowly lean forward from your hips, reaching your hands toward the floor or your feet.
- Hold for 15-20 seconds to stretch your back and hamstrings.
4. Wrist and Finger Stretch
- Extend one arm in front of you with your palm facing upwards.
- Use the opposite hand to gently pull back on your fingers, stretching your wrist and forearm.
- Hold for 10-15 seconds and repeat on the other hand.
When to Seek Help: The Role of Physiotherapy
If you experience chronic pain or discomfort due to prolonged sitting or poor posture at your desk, seeking help from a physiotherapist can be a game changer. Physiotherapy Ampang helps address musculoskeletal issues, relieving pain and improving mobility through tailored treatments, such as manual therapy, exercises, and postural adjustments. A physiotherapist can also guide you on ergonomic adjustments to prevent future injuries and promote long-term spinal health. If you are in Ampang, expert physiotherapy services are readily available at Synapse Physiotherapy Ampang, where you can receive personalized care and support, ensuring your work environment is both comfortable and safe for your body.
Conclusion: Taking Charge of Your Desk Health
Maintaining a healthy posture and taking proactive measures at your desk is essential to prevent pain and injuries. By incorporating regular breaks, practicing good ergonomics, and doing gentle stretches, you can significantly reduce discomfort and improve overall well-being. If you experience persistent pain or discomfort, consulting a physiotherapist is a wise decision to address underlying issues and prevent further damage. Take charge of your desk health today—implement these tips and don’t hesitate to seek expert help, such as Synapse Physiotherapy Ampang, for a more comfortable and injury-free workday.
Tags :

Back & Neck Pain
- Spine & Core Rehabilitation
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Group Class

Sports Injuries
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Shockwave Therapy
- Group Class

Work Desk Injuries

Pre-Post-Surgical Conditions

Scoliosis & Postural Abnormalities

Neurological Conditions

Osteoarthritis & Rheumatism
Joint degeneration and inflammation happens as the human body grows older, but that does not mean our way of life degenerates as well. Relief your joint pains with a joint effort together with your physiotherapist, who will provide pain-relief treatments and prescribe exercises for your wellbeing.

Conditions Relating To Elderly
Common conditions in the older age population include hips & knee pain, back & neck pain, osteoarthritis, rheumatism, fear of falling and many more. Aging and degeneration of bodily function is inevitable, but here at Synapse, we will help you live the best of your life.