Introduction
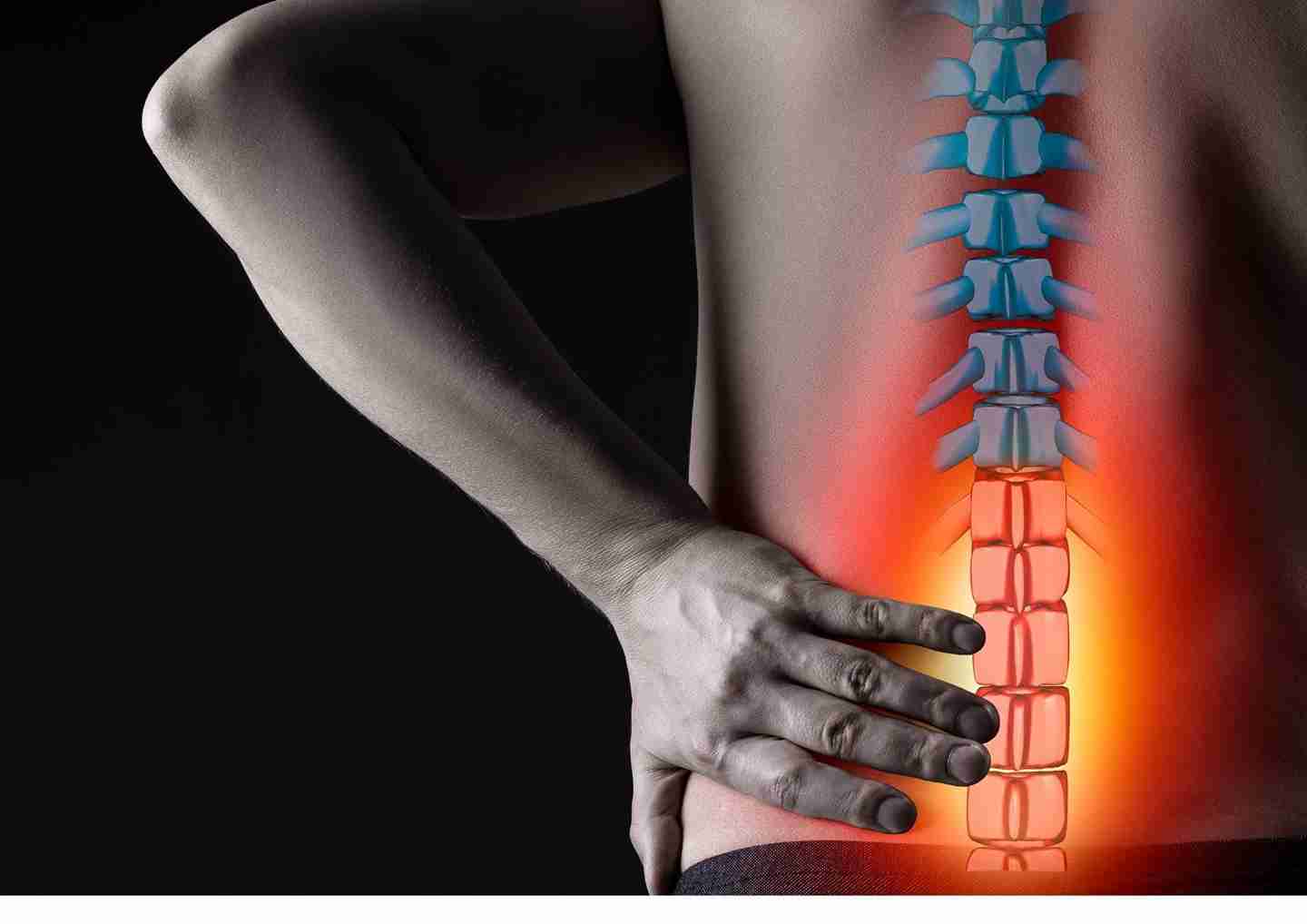
Scoliosis is an abnormal lateral curvature of the spine, most often diagnosed in childhood or early adolescence. Normally, the spine’s curves occur at the cervical, thoracic, and lumbar regions in the sagittal plane. These natural curves position the head over the pelvis and act as shock absorbers to distribute mechanical stress during movement. Scoliosis, however, involves a spinal curvature primarily in the coronal (frontal) plane. While the degree of curvature is measured on the coronal plane, scoliosis is a complex, three-dimensional problem affecting the coronal, sagittal, and axial planes.
The coronal plane is a vertical plane from head to foot, parallel to the shoulders, dividing the body into anterior (front) and posterior (back) sections. The sagittal plane divides the body into right and left halves, while the axial plane is parallel to the ground and at right angles to both the coronal and sagittal planes.
Scoliosis is defined by the Cobb’s angle of spine curvature in the coronal plane and is often accompanied by vertebral rotation in the transverse plane and hypokyphosis (reduced curvature) in the sagittal plane. These abnormalities in the spine, costal-vertebral joints, and rib cage produce a ‘convex’ and ‘concave’ hemithorax. As scoliosis becomes more pronounced, vertebral rotation increases, leading to torsion-scoliosis, which causes a prominent hump known as a gibbus.
In Malaysia, rehabilitation services are highly professional and well-equipped to treat scoliosis conditions.
Sign and Symptoms
Several signs may indicate the possibility of scoliosis, including a sideways curvature of the spine, sideways body posture, one shoulder being higher than the other, clothes not hanging properly, local muscular aches, and local ligament pain. A major concern in progressive severe scoliosis is decreasing pulmonary function. In one study, about 23 percent of patients with idiopathic scoliosis presented with back pain at the time of initial diagnosis. Idiopathic scoliosis may also affect pulmonary function due to changes in the shape and size of the thorax. Recent reports on pulmonary function testing in patients with mild to moderate idiopathic scoliosis showed diminished pulmonary function, with greater impairment observed in severe cases of spinal deformity, proximally-located curvature, and older patients.
Diagnosis
Scoliosis diagnosis in children and teenagers often occurs during routine medical examinations due to the absence of noticeable symptoms. Scoliosis chiropractors undertake a comprehensive diagnostic approach, starting with a thorough review of the child’s medical history and family background, which may uncover potential underlying medical conditions contributing to spinal curvature. Some cases are even identified through school screenings. Following this, a physical examination assesses the child’s posture, checking for any asymmetry in the trunk or shoulders. When the child bends forward, the doctor looks for signs such as one side of the rib cage appearing higher than the other, which can indicate possible scoliosis. The most definitive diagnostic tool, however, is x-ray imaging, providing detailed insights into the extent and severity of the spinal curvature. By evaluating these x-ray images, practitioners can accurately determine the severity of the condition and devise appropriate treatment strategies tailored to each individual case.
Management
Management of scoliosis depends on the severity of the curvature, measured by the Cobb angle, and the age of the patient.
Observation
For mild scoliosis, which is defined as a Cobb angle of less than 20 degrees, observation is typically recommended, especially in growing children and adolescents. Regular follow-up visits every 4-6 months are essential to monitor the progression of the curve. If the curve does not worsen, no further treatment may be necessary.
Physiotherapy
Physiotherapy can be particularly beneficial for managing mild to moderate scoliosis, defined as a Cobb angle of less than 20 degrees, or in some cases, up to 30 degrees. Physiotherapy aims to manage symptoms, improve posture, and strengthen the muscles that support the spine. Specific exercises tailored to the individual’s condition can help reduce the progression of the curve and enhance overall spinal function. By focusing on muscle balance, flexibility, and core strength, physiotherapy not only addresses the curvature but also promotes better posture and alignment, contributing to the patient’s overall well-being and quality of life.
Brace
For moderate scoliosis, especially in growing children and adolescents, orthotic specialists provide braces designed to prevent further curvature. These braces are tailored to fit each patient and are regularly adjusted to ensure effectiveness. By applying gentle pressure to the spine, braces help to maintain proper alignment and minimize the progression of the curve during periods of rapid growth. Regular monitoring and adjustments by healthcare professionals ensure that the brace continues to fit correctly and functions as intended, promoting optimal outcomes in scoliosis management.
The most common type of brace used for scoliosis is made of plastic and is contoured to conform to the body, such as the Milwaukee brace. This type of brace is designed to be nearly invisible under clothing, fitting snugly under the arms and around the rib cage, lower back, and hips. Most braces are worn day and night, and their effectiveness increases with the number of hours worn each day. Children who wear braces can usually participate in most activities with few restrictions. If necessary, the brace can be removed for sports or other physical activities.
Braces are typically removed once bone growth has ceased, which usually happens around two years after girls start menstruating, when boys begin shaving daily, or when there are no further changes in height. In general, congenital scoliotic curves are not flexible and are resistant to correction with bracing. Therefore, braces are mainly used to prevent the progression of secondary curves that develop above and below the congenital curve, which can cause imbalance. In these cases, braces may be worn until skeletal maturity is reached.
Surgery
Severe scoliosis typically progresses over time, and a specialist may suggest scoliosis surgery to reduce the severity of the spinal curve and prevent further worsening. The most common type of scoliosis surgery is spinal fusion. In this procedure, two or more vertebrae are fused together so they cannot move independently. Pieces of bone or a bone-like material are placed between the vertebrae, and metal rods, hooks, screws, or wires are used to hold that part of the spine straight and still while the old and new bone material fuses together. This stabilizes the spine and corrects the curvature to a more manageable degree.
Frequently Asked Questions (FAQs)
1. What is scoliosis?
Scoliosis is a condition where the spine curves sideways, often forming an “S” or “C” shape. It can occur at any age but is most commonly diagnosed during adolescence.
2. What are the symptoms of scoliosis?
Common symptoms include uneven shoulders, one shoulder blade more prominent than the other, uneven waist, and one hip higher than the other. Some people may also experience back pain or discomfort.
3. How is scoliosis diagnosed?
Scoliosis is diagnosed through physical exams and imaging tests like X-rays, which help determine the severity and angle of the spinal curve.
4. What are the non-surgical treatment options for scoliosis?
Non-surgical treatments include physical therapy, bracing, and exercises to strengthen the muscles around the spine and improve posture.
5. When is surgery recommended for scoliosis?
Surgery is typically recommended for severe cases where the spinal curve is greater than 40-50 degrees or if the condition is causing significant pain, functional limitations, or respiratory issues.
Conclusion
The best treatment for scoliosis depends on the Cobb angle and the severity of the patient’s condition. Typically, conservative treatments are recommended initially to prevent progression until surgery becomes necessary. At Synapse Physiotherapy, we offer professional scoliosis treatments tailored to individual needs, including physiotherapy and possibly bracing. These therapies aim to manage symptoms, improve posture, and strengthen supporting muscles to stabilize the spine and reduce curvature progression. If the condition progresses to a severe degree, surgery may be recommended to correct the spinal deformity and prevent further complications.
Tags :

Back & Neck Pain
- Spine & Core Rehabilitation
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Group Class

Sports Injuries
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Shockwave Therapy
- Group Class

Work Desk Injuries

Pre-Post-Surgical Conditions

Scoliosis & Postural Abnormalities

Neurological Conditions

Osteoarthritis & Rheumatism
Joint degeneration and inflammation happens as the human body grows older, but that does not mean our way of life degenerates as well. Relief your joint pains with a joint effort together with your physiotherapist, who will provide pain-relief treatments and prescribe exercises for your wellbeing.

Conditions Relating To Elderly
Common conditions in the older age population include hips & knee pain, back & neck pain, osteoarthritis, rheumatism, fear of falling and many more. Aging and degeneration of bodily function is inevitable, but here at Synapse, we will help you live the best of your life.