Introduction
A herniated disc in the spine occurs when the nucleus pulposus is displaced from the intervertebral space, which is a common cause of back pain. Patients with herniated disc pain often recall a specific event that triggered their discomfort. Unlike mechanical back pain, the pain from a herniated disc is often burning or stinging and may radiate into the lower extremities. In more severe cases, there may also be associated weaknesses or changes in sensation. Physiotherapy for slipped discs is important for recovery. These programs are commonly recommended to alleviate pain and restore function and neurological health in patients with symptomatic disc herniation.
Etiology
An intervertebral disc is made up of two parts: the annulus fibrosus, a tough outer ring, and the nucleus pulposus, a gel-like center. A disc herniation happens when some or all of the nucleus pulposus pushes through a tear in the annulus fibrosus.
The most common reason for disc herniation is aging. As we get older, the nucleus pulposus loses water and becomes weaker, which can lead to herniation and cause symptoms. Another common cause is trauma or injury. Other causes include connective tissue disorders and congenital issues like short pedicles. Disc herniation occurs most frequently in the lower back (lumbar spine) and the neck (cervical spine) because these areas experience more movement and stress. It is less common in the upper back (thoracic spine).
The problems caused by herniated discs come from two main factors: the disc pressing on nearby nerves and the increase in inflammatory chemicals in the area.
Herniations often occur at the sides of the disc (posterolateral), where the annulus fibrosus is thinner and less supported by ligaments. This type of herniation is more likely to press on nerve roots. A large herniation in the center of the disc can compress the spinal cord and cause more serious symptoms. The pain from a herniated disc is due to both the pressure on the surrounding ligaments and the chemical irritation from inflammation.
Sign and Symptoms
A herniated disc can present with a variety of signs and symptoms. One of the most common symptoms is severe low back pain, which can be debilitating. This pain often radiates, spreading to other areas such as the legs, a condition known as sciatica. Walking can become painful and difficult, and movements that increase pressure within the spine, such as coughing, sneezing, or straining (Valsalva maneuver), can exacerbate the pain.
Muscle-related symptoms are also frequent, including muscle spasms, tingling sensations, and weakness. In more severe cases, muscle atrophy may occur due to prolonged nerve compression. A particularly serious symptom is the loss of bladder or bowel control, which requires immediate medical attention as it indicates significant nerve compression.
Interestingly, some people with a herniated disc may be asymptomatic, experiencing no pain or discomfort. For those who do have symptoms, walking patterns can be noticeably affected. They may walk slowly and deliberately, or on their toes, to avoid pain. Additionally, the spine or trunk may appear misaligned or deviated due to muscle imbalance and pain avoidance strategies. Gait abnormalities, such as an antalgic gait (limping to avoid pain) or Trendelenburg gait (a waddling movement due to hip muscle weakness), are also common. Paraspinal muscle spasms, where the muscles along the spine tighten uncontrollably, can contribute further to pain and discomfort.
Role of physiotherapy
Acute cervical and lumbar radiculopathies due to a herniated disc are primarily managed with non-surgical treatments. NSAIDs and physiotherapy are first-line treatment modalities.
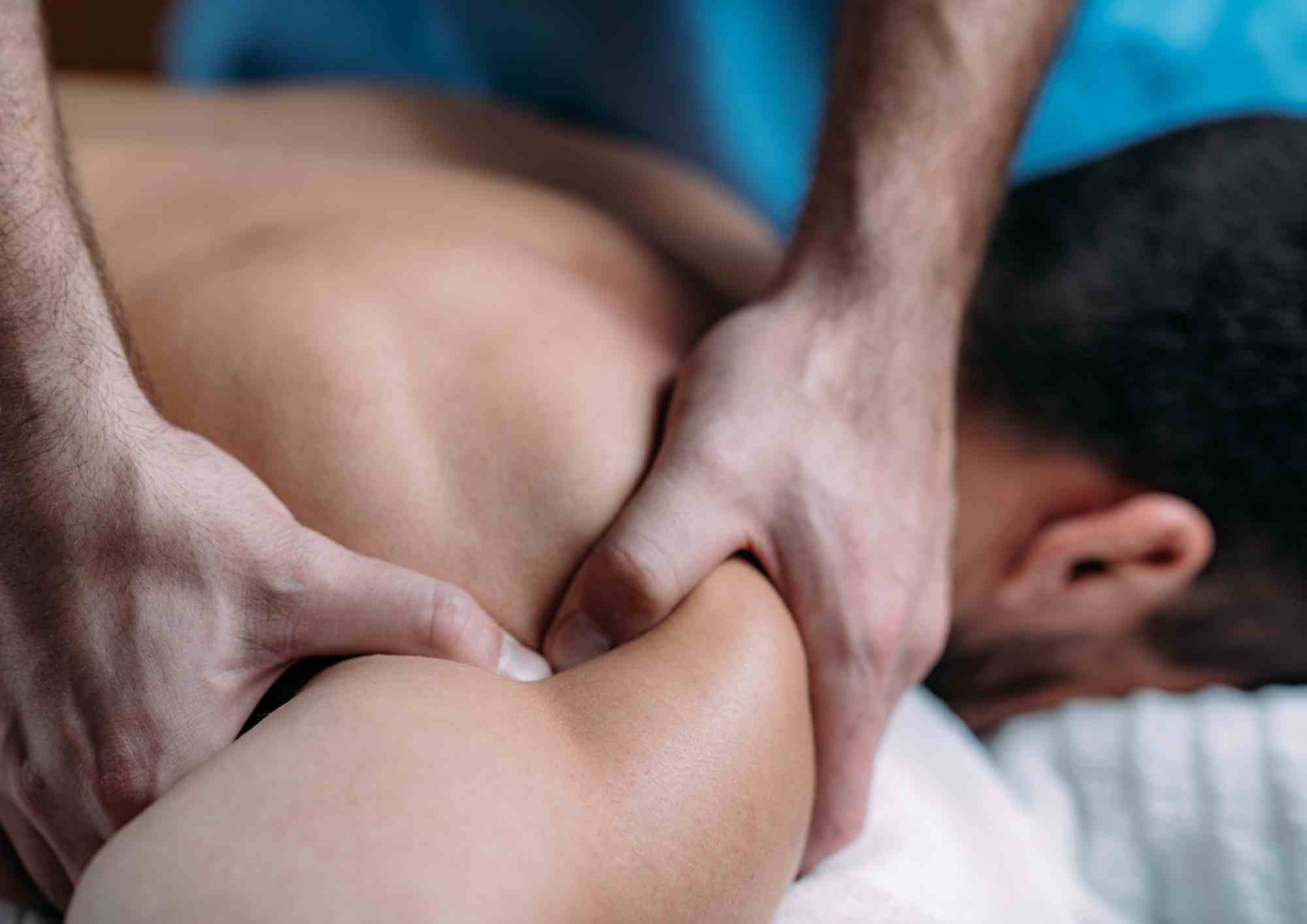
Your physical therapist plays a crucial role in reducing pain and alleviating symptoms associated with a herniated disc. They will guide you in understanding how to modify activities that may have caused the injury, allowing the healing process to commence. Various treatments and technologies may be employed by your physical therapist to manage and decrease pain.
Improving posture is another key focus. If poor posture contributes to your herniated disc, your therapist will educate you on posture correction techniques to alleviate pressure on the injured area and facilitate healing.
Restoring motion and flexibility are important aspects of therapy. Your therapist will select specific exercises and treatments to restore normal movement in stiff joints, progressing from passive motions to active exercises and stretches that you can perform independently at home or at work.
Additionally, your therapist will assess and address any muscle tightness or weakness. Stretching exercises will be prescribed to improve flexibility, while targeted exercises will be recommended to strengthen weakened or injured muscles, particularly focusing on core muscles to support your spine.
Endurance training is also integral to the recovery process. Your therapist will design a program to help you regain and enhance muscular endurance post-injury.
A customized home exercise program will be provided to complement in-clinic therapy sessions. Consistently performing these exercises as instructed by your therapist can expedite your recovery.
Your therapist will collaborate with you to set realistic goals for returning to your normal activities, whether they be work, sports, or daily tasks. Proper body mechanics will be taught to prevent further injury to your spine.
Once your pain subsides, maintaining proper posture and movement habits will be essential to prevent recurrence of symptoms and ensure long-term back health and freedom from pain. Your therapist will provide guidance on incorporating these habits into your daily routine for sustained wellbeing.
Physiotherapy treatments.
Stretching: Evidence suggests that adding hyperextension to intensive exercise programs may not significantly improve functional status or pain outcomes compared to intensive exercise alone. Similarly, combining strength training with stretching may not yield clinically relevant differences in disability and pain compared to strength training alone.
Muscle Strengthening: Strong muscles provide essential support for the spine and can better manage pain. However, caution is advised when incorporating power training into core stability exercises, as the combination of force and velocity may increase the risk of back problems and pain.
Spinal Manipulative Therapy and Mobilisation: These therapies offer short-term pain relief for acute low back pain. In cases of chronic low back pain, manipulation has been found to have a similar effect to nonsteroidal anti-inflammatory drugs (NSAIDs).
Transcutaneous Electrical Nerve Stimulation (TENS): TENS therapy can contribute to pain relief and improved function and mobility of the lumbosacral spine.
Traction: Traction therapy has shown positive effects on pain and disability in patients with intervertebral disc herniation. Some studies also suggest additional benefits when traction is combined with medication and electrotherapy.
Hot Therapies: Heat therapy increases blood flow to the affected area, delivering extra oxygen and nutrients for healing while removing waste byproducts from muscle spasms.
Cryotherapy: Cold therapy reduces spasm and inflammation, particularly in the acute phase.
Shortwave Diathermy and Ultrasound: These modalities may be used for acute and chronic conditions, with shortwave diathermy pulsed in acute conditions and continuous in chronic conditions. Ultrasound, when used as phonophoresis, increases the extensibility of connective tissues.
Frequently Asked Questions (FAQs)
1. What causes a slipped disc?
A slipped disc, or herniated disc, occurs when the gel-like center (nucleus pulposus) of an intervertebral disc pushes through a tear in the tough outer ring (annulus fibrosus). Aging, trauma or injury, connective tissue disorders, and congenital issues are common causes. Disc herniation is most frequent in the lower back (lumbar spine) and neck (cervical spine) due to increased movement and stress in these areas.
2. What are the signs and symptoms of a slipped disc?
Symptoms of a slipped disc can include severe low back pain, radiating pain into the legs (sciatica), muscle spasms, tingling sensations, weakness, and, in severe cases, loss of bladder or bowel control. Some individuals may be asymptomatic, while others may experience noticeable changes in walking patterns or gait abnormalities.
3. What is the role of physiotherapy in treating a slipped disc?
Physiotherapy for a slipped disc aims to reduce pain, alleviate symptoms, and restore function and neurological health. Treatment may involve modifying activities, improving posture, restoring motion and flexibility, addressing muscle tightness or weakness, endurance training, and providing a customized home exercise program. Physiotherapy treatments such as stretching, muscle strengthening, spinal manipulative therapy, traction, hot and cold therapies, and modalities like TENS, ultrasound, and shortwave diathermy may also be utilized.
4. What physiotherapy treatments are effective for a slipped disc?
Effective physiotherapy treatments for a slipped disc include stretching, muscle strengthening, spinal manipulative therapy, traction, hot and cold therapies, and modalities like TENS, ultrasound, and shortwave diathermy. However, caution is advised when incorporating certain exercises, such as power training, to prevent exacerbating back problems or pain.
5. How can Synapse Physiotherapy assist in recovery from a slipped disc?
Synapse Physiotherapy offers specialized services tailored to aid individuals in their recovery from a slipped disc. Whether it’s reducing pain, improving mobility, or enhancing strength and flexibility, their team provides personalized care and support to facilitate the healing process. If you’re experiencing a slipped disc or related issues, don’t hesitate to reach out to Synapse Physiotherapy for assistance in regaining your health and well-being.
Conclusion
In conclusion, physiotherapy plays a crucial role in the recovery process for disc herniation. Synapse Physiotherapy offers specialized services to aid individuals in their journey to recovery from this condition. Whether it’s reducing pain, improving mobility, or enhancing strength and flexibility, our team is dedicated to providing personalized care and support to facilitate the healing process. If you’re experiencing disc herniation or any other related issues, don’t hesitate to reach out to us for assistance. We’re here to help you regain your health and well-being.
Tags :

Back & Neck Pain
- Spine & Core Rehabilitation
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Group Class

Sports Injuries
- Strength & Conditioning Programme
- Pain Management
- Biomechanical Assessment
- Sports Physiotherapy
- Shockwave Therapy
- Group Class

Work Desk Injuries

Pre-Post-Surgical Conditions

Scoliosis & Postural Abnormalities

Neurological Conditions

Osteoarthritis & Rheumatism
Joint degeneration and inflammation happens as the human body grows older, but that does not mean our way of life degenerates as well. Relief your joint pains with a joint effort together with your physiotherapist, who will provide pain-relief treatments and prescribe exercises for your wellbeing.

Conditions Relating To Elderly
Common conditions in the older age population include hips & knee pain, back & neck pain, osteoarthritis, rheumatism, fear of falling and many more. Aging and degeneration of bodily function is inevitable, but here at Synapse, we will help you live the best of your life.